Pharmacists in Canada have become essential pillars of the healthcare system, taking on expanded roles that go far beyond dispensing medications. As our population grows and ages, and as primary care resources become increasingly strained, pharmacists are stepping up to fill critical gaps in care. Their unique combination of accessibility, expertise, and patient trust makes them well-suited to these enhanced responsibilities.
One of the most visible ways pharmacists have broadened their reach is through vaccine administration. It wasn’t so long ago that getting a flu shot or other routine vaccinations required a trip to the doctor’s office or a public health clinic. Now, across Canada, pharmacists play a key role in immunization programs. The COVID-19 pandemic underscored their importance, as pharmacists helped deliver millions of vaccine doses quickly and efficiently, often reaching communities where healthcare access was otherwise limited.
Another area where pharmacists are making a real difference is in treating minor ailments. In many provinces, they are now authorized to prescribe medications for everyday conditions such as urinary tract infections, seasonal allergies, and cold sores. This reduces the need for a lengthy wait at a doctor’s office and allows patients to receive timely treatment. Alberta, for instance, has been at the forefront, granting pharmacists the authority to prescribe independently. It’s a model that has proven effective and is gradually being embraced elsewhere.
Beyond acute issues, pharmacists are increasingly involved in the long-term management of chronic diseases like diabetes, hypertension, and asthma. Their role often includes monitoring patients, adjusting medications, and providing counseling to ensure treatments are followed correctly. Programs like Ontario’s MedsCheck allow pharmacists to conduct thorough reviews of a patient’s medication regimen, helping to prevent complications and improve quality of life. For those managing complex conditions, this kind of hands-on support can be transformative.
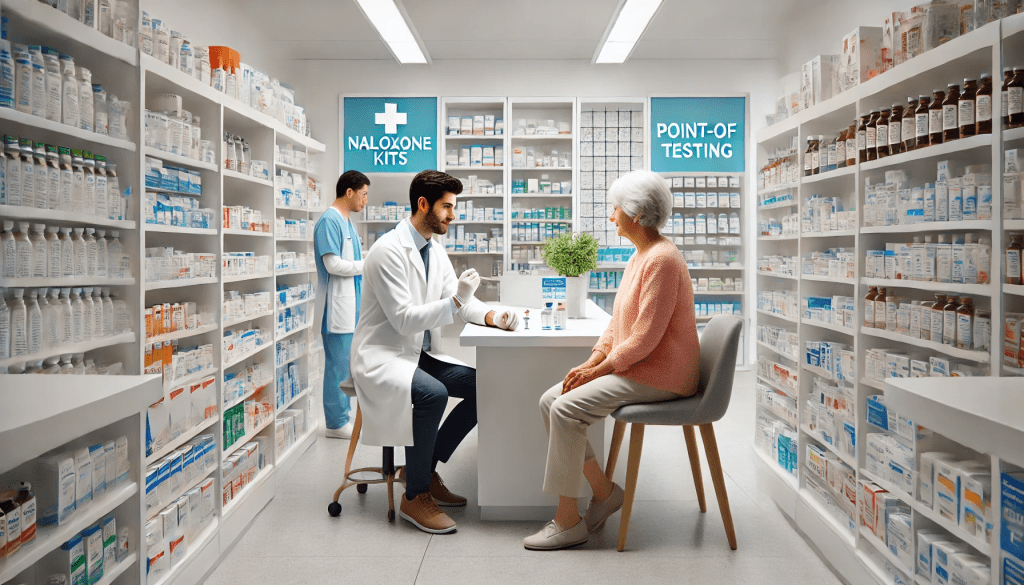
Pharmacists have also emerged as key players in addressing Canada’s opioid crisis. Many now provide naloxone kits and training, equipping individuals and families to respond to overdoses. Additionally, they support patients undergoing opioid substitution therapy, such as methadone or buprenorphine treatment, helping to reduce stigma and promote recovery. These services demonstrate the compassion and expertise pharmacists bring to some of the most challenging aspects of healthcare.
Their work extends even further, encompassing point-of-care testing for conditions like strep throat, high cholesterol, or blood sugar levels. By offering immediate results and on-the-spot advice, pharmacists enable patients to make informed decisions without delay. Nova Scotia, for example, has introduced rapid strep throat testing in pharmacies, where patients can receive a prescription on the same visit if necessary.
Mental health care is another area where pharmacists are proving invaluable. They regularly counsel patients on the proper use of psychiatric medications, monitor for side effects, and collaborate with other healthcare providers to ensure effective treatment. Saskatchewan has introduced collaborative care models that empower pharmacists to take a more active role in managing mental health conditions, a critical service given the growing demand for mental health support.
Education and preventive care are also cornerstones of pharmacists’ expanding role. They are often the first point of contact for patients seeking advice on lifestyle changes, smoking cessation, or managing the early signs of chronic illnesses. Programs in provinces like Ontario provide pharmacists with the tools and reimbursement to run smoking cessation clinics, helping countless patients improve their long-term health.
These expanded responsibilities are not without challenges. The scope of practice varies across provinces, and public awareness about what pharmacists can offer remains limited. Additionally, some services lack adequate funding, which can hinder their availability. But the potential is enormous. By empowering pharmacists further—perhaps by granting them authority to prescribe routine medications like birth control—Canada can make significant strides in improving healthcare access and outcomes.
In a system often characterized by long wait times and overstretched resources, pharmacists have emerged as trusted, knowledgeable, and accessible providers. Their ability to combine technical expertise with compassionate care is reshaping how Canadians experience healthcare, proving that pharmacists are much more than dispensers of medications—they are true healthcare partners.